
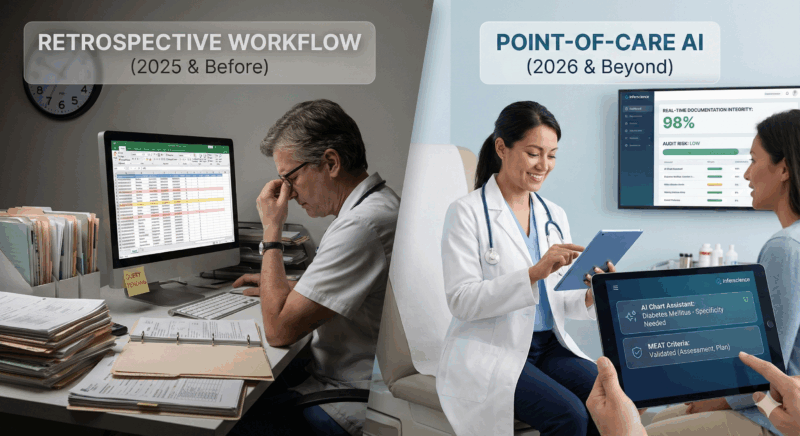
Risk adjustment is changing at a speed that traditional, retrospective workflows simply can’t match. For years, health plans and provider groups relied on manual chart reviews, post-encounter coding clean-up, and end-of-year documentation sweeps to reconcile missed diagnoses and reinforce RAF accuracy. But as compliance pressure intensifies—and as CMS tightens MEAT expectations and audit scrutiny—retrospective coding is becoming too risky, too slow, and too resource-heavy to sustain.
Manual reviews introduce delay and duplication. Providers receive queries weeks or months after a visit, often with little recollection of the clinical context. Coders are asked to interpret ambiguous documentation. Compliance teams are left to defend conditions that were never fully supported at the time of service. These gaps don’t just create operational inefficiencies—they undermine accuracy, compliance, audit defensibility, and ultimately, financial performance.
Point-of-care AI changes the equation entirely. By capturing clinical intent in real time, reinforcing MEAT criteria during the encounter, and structuring data instantly for HCC, quality, and payer alignment, point-of-care AI is becoming the new standard for risk adjustment workflows in 2026 and beyond.
Solutions like Inferscience’s AI Chart Assistant and HCC Assistant demonstrate what real-time documentation integrity looks like in practice.
The future of retrospective coding that Inferscience is working toward
Retrospective frameworks still play an important role, but they were built for a different era—one with lighter oversight, broader coding tolerance, and slower data cycles. As regulations evolve, retrospective-only approaches can no longer meet the accuracy and compliance demands of 2026.
Retrospective coding depends entirely on whatever documentation exists in the chart. If the note is incomplete, unclear, or inconsistent, coders have little recourse outside time-consuming queries that clinicians often find disruptive or frustrating. Payers and CMS now expect encounter-level accuracy, supported by complete and defensible MEAT elements. Clean-up months later simply doesn’t satisfy contemporary compliance standards.
More importantly, retrospective correction occurs too late to benefit providers or coding teams. By the time errors surface, they’ve already created downstream issues, inaccurate submissions, and avoidable audit risk.
This is exactly the gap Inferscience designed our real-time clinical validation engine to solve—capturing clinical context and MEAT support directly within the encounter, not after the fact.
Retrospective-only models aren’t just inefficient—they expose organizations to mounting compliance and audit vulnerabilities when used as the sole approach.
Rising RADV audit pressure magnifies the consequences of unsupported diagnoses. CMS now expects defensible documentation at the point of care, not explanations patched together later.
Unstructured or narrative-only documentation creates variability across providers, coders, and care settings. Coders must interpret intent rather than receiving clear, structured evidence.
Provider burnout worsens when queries arrive long after the visit, forcing clinicians to spend time revisiting encounters that are no longer fresh in memory.
Inferscience’s tools automatically convert narrative documentation into structured, audit-ready data—something retrospective coding can’t achieve.
Point-of-care AI turns the encounter into the moment where documentation accuracy actually happens. Rather than fixing incomplete notes after submission, AI assists clinicians during the visit, offering real-time clarity, completeness, and specificity.
AI solutions can surface care gaps, alerting providers to missing labs, overdue screenings, and other missing elements at the time of visit.
AI solutions can alert providers to missing MEAT elements before the chart is closed, ensuring diagnoses are supported and defensible.
They can structure data instantly, creating HCC-relevant fields, mapping meds and vitals, and aligning quality data without manual entry.
Inferscience’s point-of-care AI solutions surface MEAT elements, alert providers to care gaps, and map HCC cues without extra clicks, giving clinicians clarity and coding teams clean, structured data.
Point-of-care AI introduces capabilities that were simply impossible with retrospective systems:
This is where point-of-care AI creates an advantage retrospective coding simply cannot replicate.
Retrospective coding teams often operate without full, accurate clinical context. They must infer intent, interpret ambiguous phrasing, and second-guess what the clinician meant.
Point-of-care AI eliminates that uncertainty.
It removes coder guesswork by validating diagnoses instantly.
It reduces downstream cleanup because documentation is complete when the visit ends.
It strengthens audit trails by ensuring MEAT elements are present and traceable.
Inferscience’s portfolio directly supports these advantages:
Together, they establish a more reliable, compliant, and efficient documentation ecosystem.
Organizations adopting point-of-care AI consistently experience meaningful operational improvements:
Higher first-pass accuracy and fewer rejected codes thanks to MEAT-supported documentation.
More predictable RAF outcomes since diagnoses are captured correctly the first time.
Less administrative burden because clinicians complete documentation during the encounter instead of revisiting charts weeks later.
The shift from “corrective operations” to “proactive accuracy” dramatically reduces cost, friction, and compliance exposure.
Several technological and regulatory developments—especially those arriving in 2026—make point-of-care AI not just feasible but necessary.
TEFCA and FHIR interoperability ensure systems can exchange structured data instantly.
Clinically trained AI models understand context, nuance, and MEAT expectations.
EHR-embedded workflows remove friction and enable adoption without extra clicks or parallel systems.
Inferscience supports FHIR R4+ and integrates with major EHRs through SMART-on-FHIR and API frameworks, enabling reliability, speed, and accuracy directly in the clinical workflow.
Q1: Does point-of-care AI replace coders?
A1: No. Point-of-care AI improves the quality and completeness of documentation so coders can focus on validation, compliance, and high-value oversight rather than manual cleanup.
Q2: Is point-of-care AI just another form of ambient scribing?
A2: No. Ambient tools transcribe speech; point-of-care AI validates MEAT, clarifies diagnoses, and structures data for RAF accuracy and audit integrity.
Q3: Can point-of-care AI integrate with existing EHR systems?
A3: Yes. Inferscience integrates using FHIR R4+, SMART-on-FHIR, and REST APIs to embed seamlessly into current workflows.
Ready to move beyond retrospective coding?
Contact Inferscience for a walkthrough of our point-of-care AI solutions—and see how real-time clinical documentation can strengthen accuracy, RAF performance, and audit readiness across your organization.
Hear More at the SSN Risk Adjustment Innovations Forum
Dr. Sunil Nihalani, Founder of Inferscience, will be speaking at the upcoming SSN Risk Adjustment Innovations Forum in the session “AI in Action: Charting a Smarter Future for Coding, Quality, and Compliance.”He’ll share how plans and providers can leverage real-time AI to improve coding accuracy, reduce audit exposure, strengthen MEAT traceability, and bring clinical oversight into every step of the documentation process.If your organization is evaluating point-of-care AI, HEDIS automation, or audit-ready documentation tools, this is a session you won’t want to miss.

