Health Plans
Inferscience’s AI tools integrate with provider workflows to give health plans real-time access to accurate risk and quality data — improving care, cutting costs, and ensuring compliance.

Audit-Ready Risk Adjustment
Validate HCCs against RADV and MEAT criteria with defensible documentation to reduce recoupment risk and strengthen audit preparedness.
Improved Coding Accuracy & RAF Optimization
Surface clinically supported HCCs in real time to close gaps, reduce missed risk capture, and optimize RAF performance across the care continuum.
Higher Quality & STAR Performance
Identify and close care gaps at the point of care to improve quality outcomes, increase STAR ratings, and drive better member results.
Scalable Provider Engagement Without Workflow Disruption
Deliver actionable insights directly in the EHR, aligning payer objectives with provider workflows to improve adoption and program effectiveness.
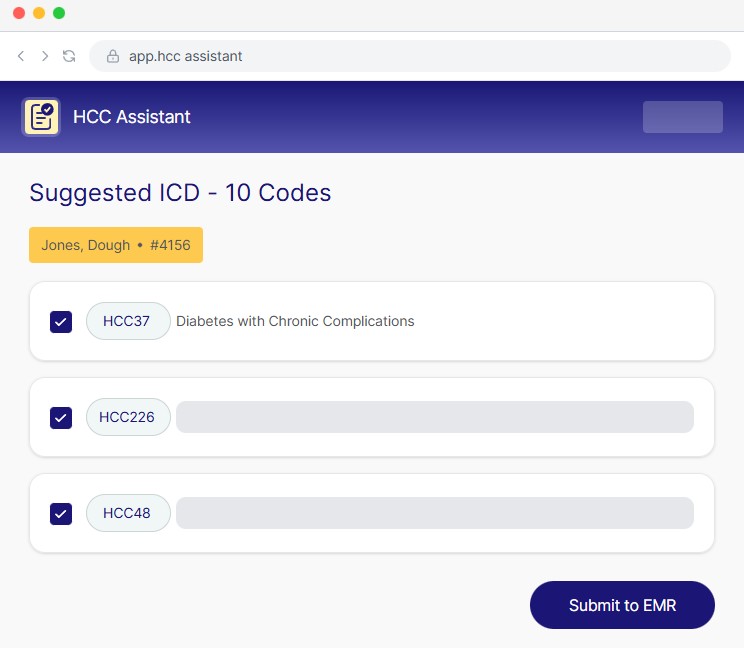
HCC Assistant helps health plans improve risk adjustment accuracy while maintaining compliance and audit readiness. Built for payer programs and embedded into provider workflows, it identifies clinically supported HCCs in real time and validates them against MEAT and RADV requirements.
By analyzing structured and unstructured data directly from the patient chart, HCC Assistant surfaces actionable coding opportunities, reduces unsupported diagnoses, and ensures risk capture is defensible

Let us help you transform your risk adjustment and quality performance with AI powered software that’s audit-ready, provider-friendly, and results-driven.