For years, many provider groups, health systems, and physician practices treated documentation integrity, quality, and risk adjustment as back-end work. Many organizations rely on retrospective chart reviews, end-of-year sweep projects, and coder-driven cleanup cycles to catch incomplete documentation or unsupported diagnoses. By the time those issues surfaced, the encounter was long over, and the opportunity to correct the record had already vanished.
This pattern didn’t come from a lack of effort or clinical skill. It came from the reality of modern practice: high volumes, busy schedules, complex EHR workflows, and clinicians forced to balance patient care with administrative pressure. Under those conditions, even the most experienced physician may miss key diagnostic criteria, overlook chronic conditions that need reactivation, or forget to close a care gap that matters for both outcomes and compliance.
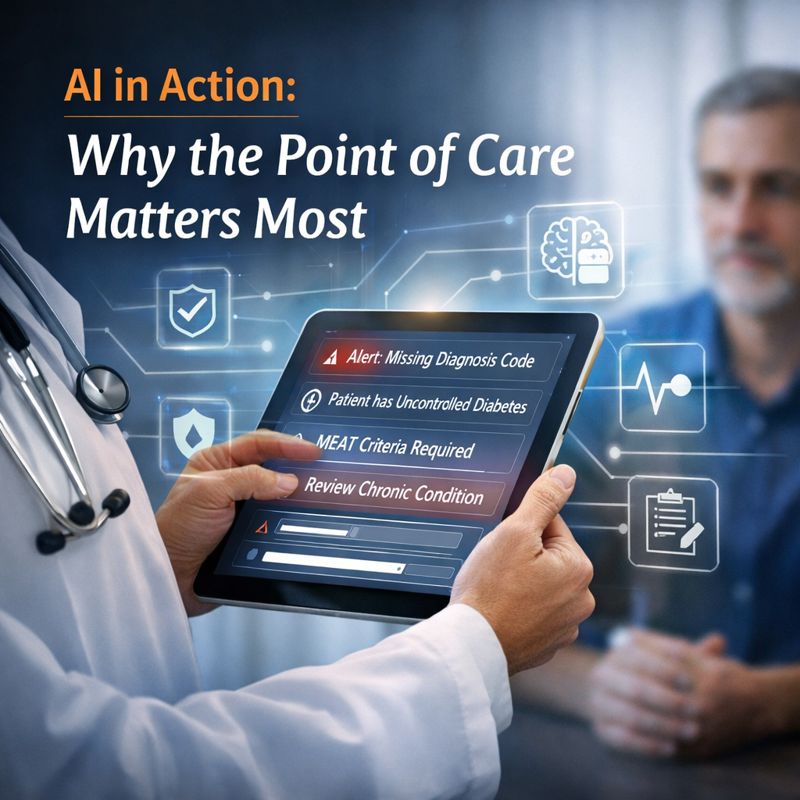
Real-time AI gives us a different path forward. If we want accuracy, audit readiness, and better patient outcomes, improvement has to happen during the encounter. Not weeks later. Not during an audit. And not after the coding team has already flagged the note.
AI belongs at the point of care because that is where documentation is created, clinical reasoning happens, and care decisions take shape.
Retrospective reviews help quantify risk, but they cannot change what happened in the exam room weeks or months earlier. When a diagnosis emerges without the supporting elements, the organization inherits downstream risk: payer friction, RADV exposure, and late-breaking queries to clinicians who barely remember the visit.
Research consistently shows that documentation variability increases as cognitive load rises, especially in fragmented EHR environments[1]. That is not a clinician problem. It is a workflow problem.
The only way to prevent the issue is to surface documentation needs before the note is signed.
When AI is present inside the visit, highlighting missing MEAT criteria, pointing out conflicting information, or signaling a chronic condition that was clinically relevant but not addressed, clinicians can take action in real time. That is the moment when it is easiest to confirm context, gather details from the patient, and document accurately.
This workflow shift is what improves diagnostic clarity, care quality, and coding accuracy simultaneously.
And importantly, it does not turn the exam room into a coding review. It simply supports the clinician’s medical decision-making process so the record reflects what actually happened.
A common concern I hear from clinicians is that point-of-care AI will add steps or slow them down. In practice, when implemented well, it does the opposite.
A well-designed AI assistant quietly organizes the clinical narrative:
Cognitive load, not clinical knowledge, is what drives documentation errors. Reducing that burden leads to better notes and better care.
One recent study in JAMA Network Open found that assistive AI reduced documentation time and improved completeness without harming clinical efficiency[2]. That is the direction we need to go as an industry.
One of the most persistent challenges in risk adjustment and quality programs is preventing unsupported diagnoses. Once a diagnosis is in the chart without adequate support, it creates risk regardless of clinical accuracy.
Point-of-care AI prevents that. By signaling when evidence is insufficient, when chronic conditions require updating, or when the clinical narrative does not align with the coded diagnosis, clinicians can make informed decisions in the moment.
This is how we lower denial rates, reduce RADV exposure, and maintain the integrity of the clinical record. Not by repairing the note months later, but by strengthening it at the source.
Historically, quality programs, risk teams, and provider operations ran in parallel lanes. Today, with the influx of AI in clinical workflows, they are interdependent. Quality measures increasingly rely on accurate condition capture. Risk programs rely on clear, complete documentation to support diagnoses. Care management depends on the same information to guide decisions.
Point-of-care AI becomes the convergence point. When documentation is complete and clinically accurate at the visit level, every downstream team benefits.
This is not just operational improvement. It is clinical improvement.
Across provider groups adopting point-of-care AI, we are seeing the same outcomes:
These results are not theoretical. They show what happens when the clinical record becomes accurate at the moment of care instead of being repaired after the fact.
The healthcare industry is saturated with tools that analyze charts after the visit. That approach can surface risk, but it cannot change the patient encounter that already occurred.
The next stage of AI in medicine will not be about cleanup. It will be about integration.
AI must move into the clinician’s workflow, not sit outside it. It must support the medical decision-making process, not interfere with it. And it must reduce friction, not create another inbox or queue for clinicians to manage.
If we want documentation accuracy, clinical clarity, and stronger compliance, the point of care is where the transformation has to happen. That is where AI can make the most meaningful impact for clinicians, for patients, and for the organizations responsible for their outcomes.
About the Author
Dr. Sunil Nihalani is the Founder and CEO of Inferscience and a practicing physician with more than two decades of experience in internal medicine and gastroenterology. Frustrated by fragmented, poorly integrated clinical decision support tools, he founded Inferscience in 2014 to help reduce administrative burden, streamline clinical workflows, and improve patient care through technology.
Today, Dr. Nihalani leads the development of AI-powered solutions that support accurate documentation, compliant risk adjustment coding, and better outcomes for providers and health plans nationwide. His work focuses on embedding AI into clinical workflows in ways that enhance decision-making without disrupting care delivery.
Dr. Nihalani will be speaking at the SSN Risk Adjustment Innovations Forum, January 21–22, 2026, where he will present AI in Action: Charting a Smarter Future for Coding, Quality, and Compliance, sharing practical insights on how organizations can operationalize AI while maintaining clinical integrity and audit readiness.