
Imagine trying to manage a healthcare organization without a clear idea of how much each patient’s care is likely to cost. Not only would it be difficult to manage long-term budgets or predict appropriate remuneration for physicians – it would create ongoing problems for the delivery of fair and accurate insurance reimbursements.
That is why hierarchical condition category (HCC) risk adjustment is such a popular topic in healthcare management today. In the United States, Medicare Advantage plans now cover nearly one-third of all Medicare members, making it more important than ever for healthcare firms to pay attention to the HCC risk adjustment codes model.
The HCC risk adjustment model is used to predict anticipated costs for Medicare Advantage beneficiaries by CMS, and the results have a direct impact on the compensation healthcare organizations receive. The model uses hierarchical condition category (HCC) codes to calculate a patient-specific risk adjustment factor (RAF) score – which are applied to capitation payments for Medicare Advantage plan members.
As the American Academy of Family Physicians states: “hierarchical condition category coding helps explain patient complexity and construct a picture of the full patient,” assisting in the proper measurement of quality and cost. HCC coding and risk adjustment accuracy can therefore have a substantial impact on the financial viability and service delivery of healthcare organizations.
Patient-specific Risk Adjustment Factors (RAFs) are calculated using data from the HCC model and applied to capitation payments for Medicare Advantage plan members. As stated by the American Academy of Family Physicians, “hierarchical condition category coding helps explain patient complexity and construct a picture of the full patient,” assisting in the proper measurement of quality and cost. HCC coding and risk adjustment accuracy can therefore have a substantial impact on the financial viability and service delivery of healthcare organizations.
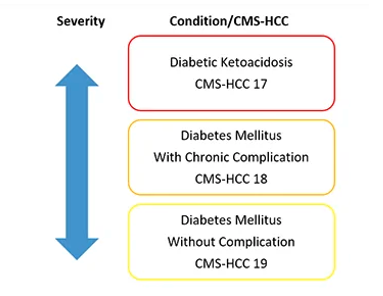
Hierarchical condition categories are based on the fact that different illnesses within the same family (or group) might have varying degrees of severity. Thus, the most severe takes precedence over the others and be used in calculation of patient’s risk score. As in the case of Diabetes as seen above, and in the chart below you can see how certain HCC codes have different risk scores attached to them. The following is an example of HCC codes in the chart of a 70 yr old woman who lives in an institution with type 2 diabetes, diabetic foot ulcer and hypertensive heart disease.
| ICD 10 CODE | HCC DESCRIPTION | CMS HCC CATEGORY | HCC RISK SCORE |
| E11.621 | Type II diabetes with foot ulcer. | HCC18 | 0.307 |
| I11.0 | Hypertensive heart disease | HCC85 | 1.351 |
In addition to diagnoses, certain demographic factors are also considered in calculating the RAF. These include:
Using this article as a guide, we’ll go through the fundamentals of risk adjustment models and our five recommendations to Improve HCC Coding and Risk Adjustment.
Accurate data management is a key step in improving the HCC coding sector, involving a collaborative effort of key sector players. It is therefore important that a structure is set up in such a way as to include a multidisciplinary team that would be responsible for enhancing documentation and HCC coding accuracy.
ACO team members, doctors, clinic managers, operations, and medical coders could all be included in this working group. This multidisciplinary effort could then be geared towards spearheading a working approach to drive improvements through five key steps:
As a result of years of data entry into an EMR, many healthcare organizations now have a large problem list that is likely inaccurate. Duplicate and inactive diagnoses must be eliminated, key areas with discrete data identified, and a diagnosis preference list used to include HCC suffix codes and RAF values as well as prioritize results are all part of the process of ensuring an accurate problem list.
Identifying patients with chronic illnesses who haven’t been seen in a calendar year is the first part of the process. If that’s the case, the next step is to try to bring them in to be seen (which may be more logistically tasking). You can achieve this with:
Clinicians must be trained along the way, as this is an unfamiliar and counterintuitive practice. In terms of teaching, the most crucial aspect to convey to physicians is that accuracy is more important than a precise score. Clinicians can benefit from group education on the importance of specificity, which can be beneficial both clinically and financially:
Accurate HCC coding cannot be achieved without both education of clinicians and the integration of suitable coding into everyday clinical encounters. This should include:
Understanding the main data elements in the healthcare ecosystem will help accurately depict risk scores at both the individual and population levels. For better patient care documentation and the detection of potentially incorrect disease documentation, administrative, clinical, and auxiliary data informs your risk adjustment accuracy program.
In case of poor data management, one could end up with wrong HCC risk adjustment coding, incorrect remuneration for quality of care, and an elevated audit risk if several data streams are not utilized.
The most important responsibility assigned to the group is to keep a watch on the results and seek places where they might be made better in the future. The workgroup can present stakeholders with:
Identifying possible areas for improvement follows data collection and dissemination among stakeholders, which is the next stage after that. Unresolved chronic conditions affecting specific populations can be investigated to aid in detecting them.
Audit preparedness in addition to the above is crucial. Organizations should make it a priority to equip their risk adjustment accuracy program with the tools needed to accurately assess the health risks of their members, hence lowering their overall risk exposure. Automated analytics solutions that give coders documented clinical evidence of accurate coding between the medical record and claim codes are an important part of a risk adjustment accuracy program designed for success. By utilizing these technologies, the reconciliation process can be sped up and the associated risk can be reduced.
Automating manual processes is essential as it allows for more and more patient records to be processed efficiently and accurately by coding teams on a bigger scale. A key component of an automated process is making it part of your coders’ daily routine, which increases productivity by a factor of 10. In order to deal with the growing number of MA enrollees, healthcare providers who use natural language processing technologies in their operations will have a leg up.
Key Points to note in improving HCC coding accuracy and risk adjustment:
Changing how healthcare organizations document and categorize chronic diseases can help them collect more thorough diagnoses, leading to greater and more appropriate compensation as well as better healthcare delivery for complicated patient populations. As the number of Medicare Advantage beneficiaries grows, healthcare facilities are finding it harder to stay financially sustainable. Patients with chronic illnesses should be examined annually, and decision-support and EMR optimization should be improved. A great way to achieve EMR optimizations is with integrations to your EMR, the HCC Assistant is a great software tool that integrates with a variety of EHRs and suggests HCC risk adjustment codes at the point of care.
HCC Assistant uses natural-language processing (NLP) to take the weight off yoru providers’ backs. The tool delivers HCC coding recommendations at the point-of-care, with a 97% accuracy rate – helping it increase the average provider’s RAF scores by 35%. Book a Demo.
Sunil Nihalani, M.D is the founder and CEO of Inferscience. He spent over 10 years practicing internal medicine and gastroenterology before shifting his focus to tech – building solutions that are trusted by leading healthcare providers to streamline risk adjustment workflows and improve the accuracy of HCC coding.