
This article examines ten pivotal medical technology advancements that are currently revolutionizing healthcare. These include:
Each advancement is substantiated by evidence demonstrating enhanced patient outcomes, increased operational efficiency, and the promise of personalized medicine. This illustrates the profound impact these technologies are having on the healthcare landscape.
The rapid evolution of medical technology is reshaping the healthcare landscape, introducing groundbreaking innovations that promise to enhance patient care and operational efficiency. From artificial intelligence that streamlines coding processes to wearable devices that monitor health in real-time, these advancements are not merely improving outcomes; they are revolutionizing the way healthcare is delivered.
However, as these technologies emerge, critical questions arise regarding:
What does the future hold for these transformative technologies, and how will they redefine the standards of care in the coming years?
The Inferscience HCC Assistant leverages medical technology advancements to harness the power of artificial intelligence for automating the collection and analysis of clinical data, providing timely coding suggestions right at the point of care. This revolutionary approach, driven by medical technology advancements, not only boosts coding accuracy but also alleviates the administrative burden on medical providers, enabling them to devote more attention to patient care while maximizing funding from Medicare Advantage contracts.
Seamlessly integrated into electronic health records (EHRs), the HCC Assistant exemplifies medical technology advancements as an essential tool in medical coding, enhancing compliance and significantly elevating Risk Adjustment Factor (RAF) scores. Organizations that have adopted medical technology advancements report an impressive increase of up to 35% in RAF scores, highlighting the effectiveness of AI in refining coding practices.
Furthermore, the integration of natural language processing (NLP) tools, as part of medical technology advancements, has led to productivity gains of 11-30%, underscoring the profound impact of AI on both medical coding accuracy and operational efficiency. As the healthcare landscape evolves, the HCC Assistant is at the forefront, utilizing medical technology advancements to transform coding procedures and ensuring that practitioners can adeptly navigate the complexities of HCC coding with confidence.

AI diagnostics leverage machine learning algorithms to analyze vast medical data, resulting in faster and more accurate diagnoses. These sophisticated systems can handle extensive datasets from diverse sources, including imaging and laboratory results, empowering medical professionals to make informed decisions. By significantly reducing the time required for diagnosis, AI diagnostics not only improve outcomes for patients but also enhance the overall efficiency of clinical practice.
Medical technology advancements allow providers to dedicate more time to patient care, addressing the pressing need for efficiency in an environment where 41% of medical professionals report spending over four hours daily on administrative tasks. As we approach 2025, nearly 98% of medical leaders expect to integrate AI into some aspect of diagnostics, reflecting a strong trend towards medical technology advancements in clinical workflows.
The benefits of machine learning in medical data analysis are evident, with healthcare systems achieving up to a 50% reduction in hospital readmissions through predictive analytics. This evolution in diagnostics is not merely a technological advancement; it represents a paradigm shift in the delivery of medical services, ultimately leading to improved care for patients and enhanced operational efficiency through medical technology advancements.
Wearable medical devices, such as smartwatches and fitness trackers, are transforming the landscape of continuous health monitoring due to medical technology advancements. These innovative devices meticulously track vital signs, physical activity, and sleep patterns, generating invaluable data that can be seamlessly shared with healthcare providers. This real-time monitoring empowers early intervention for potential health issues, fostering a proactive approach to health management. Notably, studies indicate that 86% of patients believe that wearable medical devices significantly enhance health outcomes, underscoring their effectiveness in improving patient care.
Moreover, the data collected not only aids in monitoring but also enhances coding accuracy and supports reimbursement claims, ensuring compliance with regulatory requirements. Inferscience’s HCC Assistant exemplifies how technological innovations can further streamline these processes by employing advanced natural language processing (NLP) to optimize HCC coding workflows. By integrating claims analysis insights directly into the EHR, providers can maximize workflow efficiency and secure the maximum funding from Medicare Advantage contracts.
The market for wearable medical devices is projected to reach approximately $156 billion by 2032, with a remarkable compound annual growth rate (CAGR) of 17.8% during the forecast period from 2025 to 2032. This growth underscores the increasing importance of incorporating medical technology advancements into medical systems to enhance individual health outcomes and simplify administrative procedures. Additionally, interoperability protocols such as HL7 and FHIR are essential for facilitating data exchange and mitigating fragmentation, thereby enhancing the effectiveness of wearable devices in healthcare settings.
However, it is paramount to address the escalating concerns surrounding data privacy and security, as these issues profoundly impact user trust and adoption rates.
Robotic surgery utilizes sophisticated robotic systems, which are examples of medical technology advancements, to assist surgeons in executing intricate procedures with remarkable precision. These minimally invasive methods lead to smaller incisions, decreased blood loss, and quicker recovery periods for individuals. For instance, robotic-assisted laparoscopic hysterectomy accounted for 60.8% of hysterectomies in the U.S. in 2018, showcasing the growing adoption of these technologies. The da Vinci Surgical System, a leader in this field, has been utilized in over 8.5 million surgeries worldwide, with more than 6,730 systems deployed globally by 2021, demonstrating its effectiveness across various specialties, including urology and gynecology.
The benefits of robotic surgery extend beyond individual outcomes; they also result in considerable cost reductions for healthcare providers. Studies indicate that robotic-assisted surgeries can reduce hospitalization costs by approximately $3,000 compared to traditional laparoscopic procedures, despite the initial higher costs associated with robotic systems. Furthermore, robotic surgery has been linked to a 2.2% reduction in complications and a decrease in length of stay, enhancing overall surgical efficiency. The typical duration of stay for individuals undergoing robotic-assisted surgery is 2.9 days, in contrast to 3.9 days for laparoscopic surgery, emphasizing the effectiveness of these methods.
As Dr. Johannes Kratz observes, ‘Instrumentation is becoming increasingly advanced, and robotic surgery may assist in transforming open procedures into minimally invasive ones, making that a more attractive choice for individuals.’ This sentiment reflects the ongoing evolution of surgical techniques, where medical technology advancements, such as robotic systems, not only meet compliance with surgical standards but also align with reimbursement protocols, making them a viable option for medical providers aiming to improve both patient care and operational efficiency. Notably, robotic surgery now accounts for about 22% of surgeries performed in the United States, indicating its growing prevalence in surgical practices. However, the financial implications remain significant, as the average cost for robotic-assisted surgeries is approximately 25% higher than conventional laparoscopic surgery, necessitating careful consideration by healthcare CFOs.
Genomic editing methods, particularly CRISPR, have revolutionized personalized medicine by enabling precise modifications to DNA. This groundbreaking capability facilitates targeted interventions that directly address specific genetic mutations, leading to significantly improved treatment outcomes for various conditions, including genetic disorders and certain cancers. Currently, CRISPR-based therapies are under investigation in over 100 clinical trials globally, highlighting their potential to customize treatments based on individual genetic profiles. Additionally, the field boasts more than 10,000 publications on CRISPR applications and possibilities, underscoring the extensive research that supports this innovative area.
This level of customization not only enhances treatment efficacy—evidenced by CRISPR-mediated gene editing success rates ranging from 50% to 90% across different experimental setups—but also brings forth essential compliance and ethical considerations that healthcare providers must meticulously address. As the global CRISPR market is projected to grow from USD 3.2 billion in 2023 to USD 15 billion by 2033, with the market in India expanding from USD 3.19 billion in 2017 to USD 6.28 billion by 2022, the implications of these advancements are profound. Furthermore, ethical guidelines have been established by over 50 countries to tackle concerns related to genomic editing, emphasizing the necessity for responsible application and oversight within clinical environments.

Augmented and virtual reality (AR/VR) innovations are revolutionizing surgical training and planning as a result of medical technology advancements, providing immersive experiences that empower surgeons to rehearse procedures in a risk-free environment. This hands-on approach markedly enhances their skills and confidence.
Studies indicate that VR training can elevate performance by up to 230% compared to traditional methods, as evidenced by a UCLA study. Furthermore, AR tools significantly assist during surgeries by projecting critical information directly onto the surgical area, thereby boosting accuracy and improving outcomes for patients.
For example, AR tools like AccuVein project a map of veins onto a patient’s skin, facilitating precise IV placements. As medical technology advancements become increasingly integrated into medical education, adherence to training standards and accreditation requirements will be essential for healthcare institutions to ensure effective implementation and maximize the benefits of these innovative solutions.

Medical technology advancements, especially in neurostimulation technologies like deep brain stimulation (DBS), are revolutionizing treatment options for conditions such as Parkinson’s disease and chronic pain. These devices deliver targeted electrical impulses to specific regions of the nervous system, effectively alleviating symptoms and significantly enhancing individuals’ quality of life. However, it is essential to recognize that care gaps can impede the effectiveness of such advanced treatments. For instance, if individuals do not receive timely follow-ups or necessary screenings, their eligibility for therapies like DBS may be compromised, ultimately affecting their health outcomes.
Recent medical technology advancements in DBS have demonstrated remarkable efficacy, with studies revealing that 80.9% of individuals receiving 10,000 Hz stimulation therapy achieved over 50% pain relief. Furthermore, the long-term benefits of DBS, supported by medical technology advancements, are evident, as 83% of participants in a three-year follow-up reported clinically significant improvements in their condition. As the landscape of neurostimulation continues to evolve, understanding the compliance and reimbursement systems for these therapies is crucial for healthcare professionals. This knowledge ensures that individuals have access to these innovative treatments, ultimately enhancing their overall health results.
Healthcare providers should consider integrating DBS into their treatment protocols while also addressing care gaps to improve client care and outcomes.
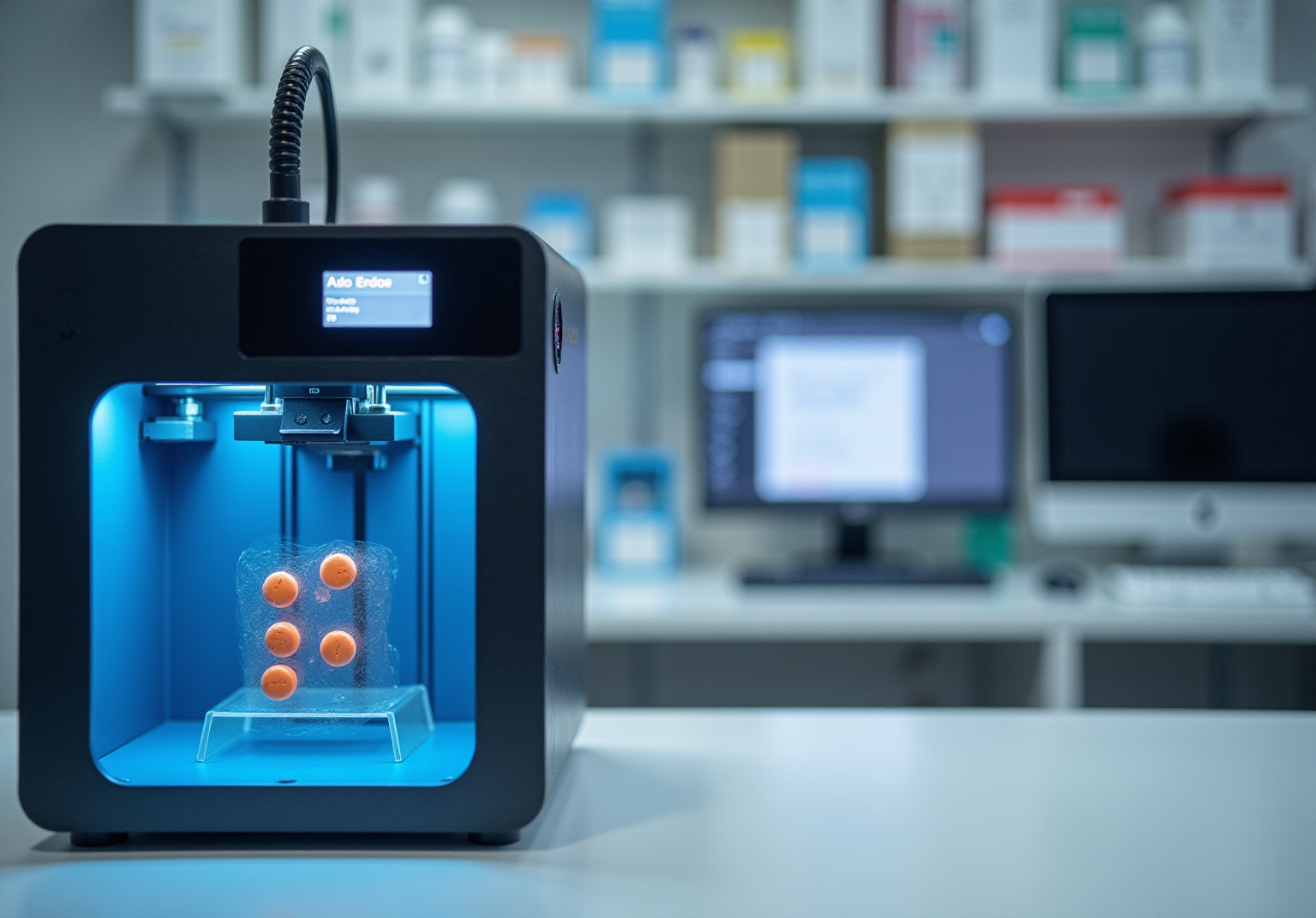
3D printed drugs exemplify medical technology advancements that transform pharmaceutical technology, enabling the development of personalized medication formulations tailored to individual requirements. This innovative method allows for the creation of medications with varying dosages and customized release profiles, significantly enhancing adherence and therapeutic effectiveness. For instance, 3D printing facilitates the production of dual-drug tablets that combine multiple active components, simplifying complex medication regimens for individuals managing chronic conditions such as diabetes and hypertension.
However, the integration of 3D printed medications into healthcare systems requires meticulous attention to regulatory and compliance frameworks. With the FDA beginning to approve 3D-printed medications, including the inaugural prescription drug, Spritam, the establishment of clear guidelines is paramount to ensure safety and efficacy. The challenges associated with maintaining consistent quality and precise dosages for each printed product further underscore the necessity for robust quality assurance mechanisms.
Furthermore, medical technology advancements related to 3D printed drugs can significantly enhance operational efficiencies for payers. By facilitating personalized medication regimens, these technologies can alleviate the administrative burden tied to managing complex prescriptions while improving health outcomes. As payers navigate the intricate regulatory landscape, investing in FHIR-compliant APIs will be vital for streamlining processes and fostering partnerships with providers, ultimately yielding a competitive edge in the healthcare market. The potential of 3D printing in pharmaceuticals transcends mere technological advancement; it heralds a shift towards personalized medicine, where treatment plans can be customized to meet the distinct needs of each individual, thereby enhancing health outcomes and overall satisfaction.
Biotechnology is revolutionizing the restoration of auditory and visual functions for individuals with sensory impairments. Innovations such as cochlear implants and retinal prostheses are not only enabling individuals to regain lost functions but are also significantly enhancing their quality of life.
For instance, studies indicate that:
As medical technology advancements continue to evolve, medical providers must navigate crucial compliance and reimbursement considerations to ensure individuals have access to these life-changing technologies. The substantial effect of hearing impairment on mental well-being, such as increased instances of depression and cognitive deterioration, further highlights the wider consequences of unaddressed hearing loss on medical expenses.
The integration of medical technology advancements and other innovative solutions not only enhances outcomes for individuals but also presents new challenges for healthcare systems regarding funding and support services, emphasizing the necessity for ongoing dialogue and adaptation in the healthcare landscape.

The emergence of artificial ovaries signifies a groundbreaking advancement in reproductive medicine, showcasing medical technology advancements that instill renewed hope for women facing infertility. These bioengineered ovaries are meticulously crafted to mimic the natural function of ovaries, potentially restoring hormonal balance and fertility for patients impacted by conditions such as cancer treatments or premature ovarian failure. Recent strides in medical technology advancements, particularly through the application of biocompatible scaffolds and stem cells, have enabled the development of synthetic ovaries capable of supporting follicle maturation and hormone production.
As we approach 2025, the ramifications of these innovations are increasingly apparent. For example, research indicates that artificial ovaries can facilitate the generation of oocytes, with promising outcomes documented in animal models. Notably, over 100 children have been conceived following ovarian tissue transfers, and a cumulative total of 318 women worldwide have undergone these procedures, underscoring the transformative potential of these methods in reproductive health. Additionally, the incorporation of growth factors such as VEGF and bFGF within artificial ovaries has demonstrated a capacity to enhance follicle survival and vascularization, which are essential for restoring ovarian function.
The implications for reproductive medicine are profound due to medical technology advancements. Artificial ovaries not only provide a compelling alternative to conventional fertility treatments—often characterized by high costs and emotional strain—but also present a viable option for young women experiencing infertility as a result of cancer therapies. However, it is crucial to acknowledge that further research is necessary to substantiate the clinical relevance of these medical technology advancements. As Dr. Richard Anderson emphasized, an artificial ovary capable of supporting the development of follicles and eggs would hold significant scientific value. As research advances, prioritizing ethical considerations and regulatory compliance will be vital to ensure the safe implementation of these technologies in clinical environments. The ongoing evolution of artificial ovaries has the potential to redefine fertility preservation strategies, offering women the chance to conceive naturally while regaining hormonal balance without the associated risks of long-term hormone therapies.

The advancements in medical technology are fundamentally reshaping the healthcare landscape, driving significant improvements in patient outcomes and operational efficiencies across various domains. Innovations such as AI-driven diagnostics enhance accuracy while alleviating administrative burdens. Moreover, wearable devices facilitate continuous health monitoring, positioning these technologies at the forefront of healthcare delivery transformation. The integration of robotic surgery, genomic editing, and augmented reality not only streamlines processes but also empowers healthcare professionals to deliver personalized care tailored to individual patient needs.
Key insights highlighted in the article underscore the profound impact of these technologies:
As the healthcare industry evolves, embracing these technological advancements is essential. Stakeholders must prioritize the integration of innovative solutions while addressing compliance and ethical considerations to ensure these advancements translate into tangible benefits. The potential to enhance patient care and operational efficiency through these technologies is substantial. Proactive engagement with these developments will be crucial for shaping the future of healthcare.