
The article “7 Key Insights on Meat Coding Guidelines for HCC Success” captures the critical strategies and tools essential for effective Hierarchical Condition Category (HCC) coding, a pivotal element for optimizing healthcare funding and ensuring compliance. It underscores the necessity of leveraging advanced technologies such as AI and NLP to enhance coding accuracy. Furthermore, it advocates for the implementation of MEAT criteria to ensure thorough documentation and emphasizes the importance of conducting regular audits. These practices are vital for maintaining compliance and elevating overall coding standards.
In the evolving landscape of healthcare, the imperative for accurate Hierarchical Condition Category (HCC) coding cannot be overstated. It is essential for optimizing reimbursement and enhancing patient care. The integration of advanced technologies, such as artificial intelligence and natural language processing, is revolutionizing this process. Tools like the Inferscience HCC Assistant are streamlining coding, enabling healthcare providers to significantly improve accuracy and efficiency at the point of care.
As organizations navigate the complexities of Medicare Advantage funding, it becomes crucial to grasp the importance of comprehensive documentation, adherence to MEAT criteria, and the implementation of innovative solutions. This article explores the transformative impact of these technologies and practices on HCC coding. It highlights the challenges faced by healthcare providers and outlines the strategies that can lead to improved financial outcomes and heightened patient satisfaction.
The Inferscience HCC Assistant revolutionizes the gathering and examination of clinical data, delivering prompt classification recommendations right at the point of care. This cutting-edge tool integrates seamlessly with electronic patient records (EHRs), providing real-time classification assistance that significantly alleviates the administrative burden on medical staff. By leveraging advanced artificial intelligence and natural language processing, the HCC Assistant not only enhances the accuracy of HCC classification but also empowers providers to concentrate more on patient care while optimizing funding from Medicare Advantage agreements.
As we look to 2025, the AI in medical documentation market is poised for remarkable growth, with a striking 78% of users reporting improved comprehension of their lab results through AI-driven explanations. This statistic underscores the transformative potential of AI tools like the HCC Assistant in enhancing accuracy and efficiency in programming, ultimately leading to improved patient outcomes and financial performance for medical organizations.
Moreover, Inferscience’s API solution enhances healthcare interoperability by enabling seamless HCC data exchange among providers, payers, and third-party vendors. This API allows payers or third-party vendors to integrate it with their existing systems, facilitating the upload of claims files (PDF or CCDA documents). The data is then extracted and analyzed using intelligent rules, delivering insights in JSON format that can be accessed in seconds. Such comprehensive access to patient data drives better-informed decisions, ensuring precise documentation from the outset of patient visits.
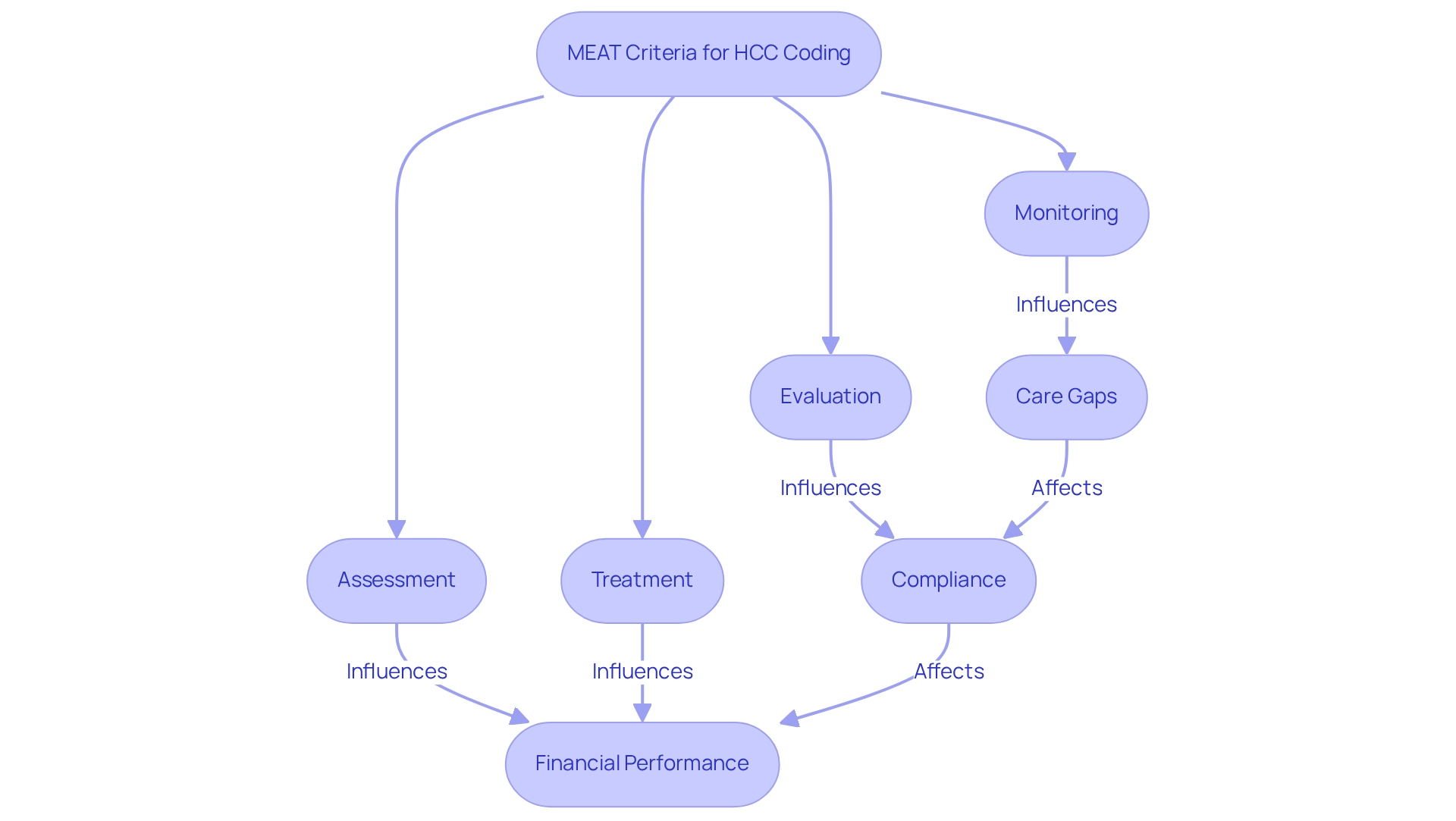
The MEAT criteria are essential for effective HCC classification, ensuring that every diagnosis is thoroughly documented through monitoring, evaluation, assessment, and treatment during patient encounters. A ‘care gap’ refers to instances where patients have not received necessary screenings or follow-ups, which can hinder optimal patient outcomes. This comprehensive documentation not only simplifies the programming process but also substantiates the medical necessity of services rendered, which is vital for compliance with Medicare regulations.
In 2025, adherence to MEAT criteria is more critical than ever, as it directly impacts reimbursement accuracy and financial performance. Statistics suggest that organizations utilizing MEAT-enabled programming solutions have experienced substantial enhancements in compliance rates, with Community Health Network (CHN) attaining a follow rate for HCC alerts of 64%, greatly surpassing the industry standard of 40-50%. Moreover, recognizing care gaps can improve the efficiency of HCC classification.
Successful documentation practices, supported by regular audits and reviews, are crucial in maintaining high standards of accuracy and efficiency in HCC coding. As John Pitsikoulis observes, the incorporation of strong documentation practices is essential for boosting revenue and guaranteeing compliance in today’s intricate medical environment. Additionally, leveraging AI and natural language processing (NLP) tools can specifically address the causes of care gaps by optimizing risk adjustment workflows, reducing human error, and ultimately improving Medicare Advantage funding outcomes.
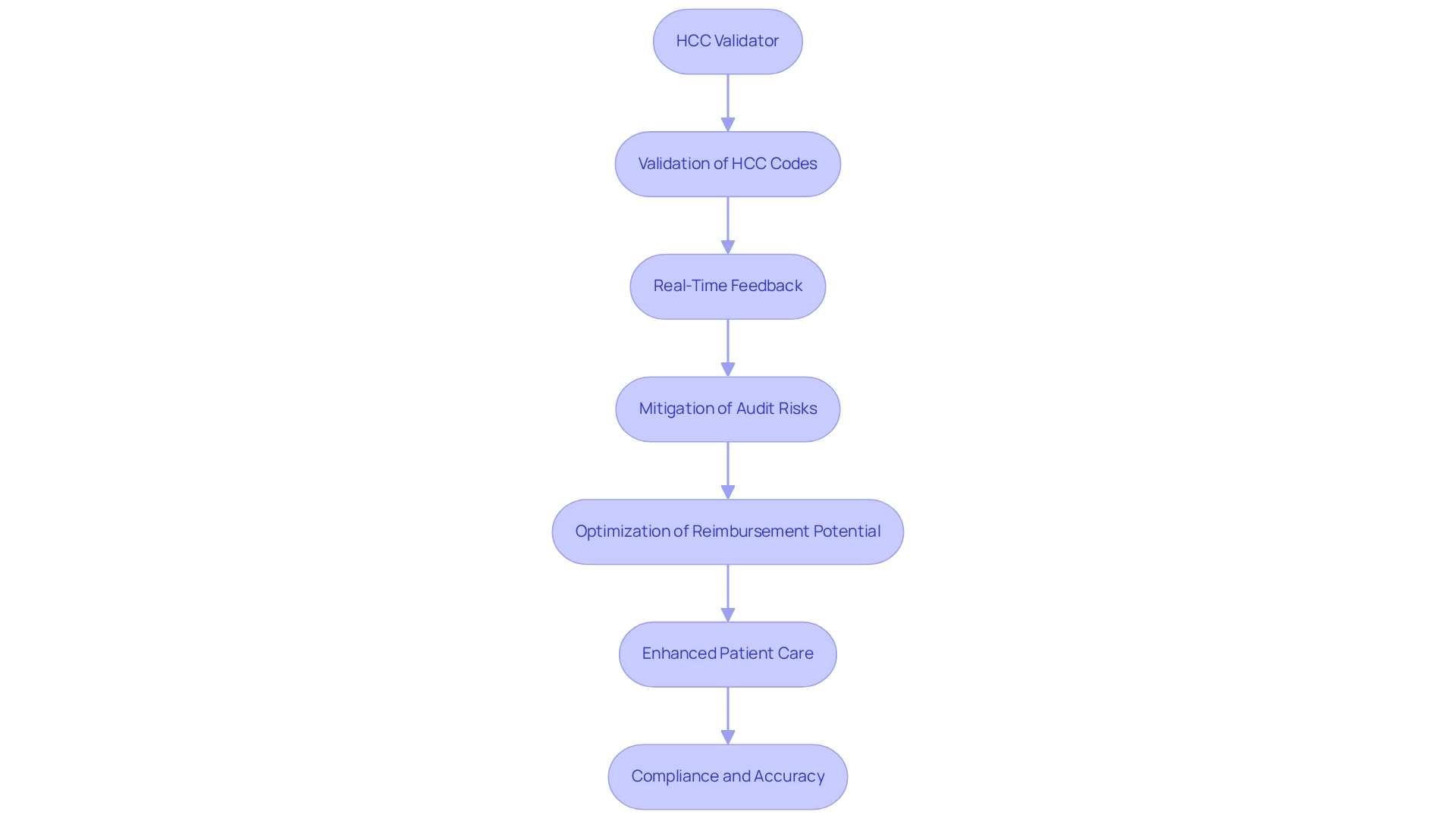
The HCC Validator harnesses advanced natural language processing technology to rigorously validate HCC codes against the MEAT criteria. This innovative tool provides coders with real-time feedback, ensuring compliance with documentation standards. By accurately assigning codes, the HCC Validator not only mitigates the risk of costly audits and penalties but also optimizes reimbursement potential for healthcare organizations, significantly impacting their financial viability within the Medicare Advantage landscape.
As we look to 2025, the impact of natural language processing on HCC classification compliance is increasingly evident. Organizations that adopt such technologies report notable improvements in accuracy. A recent validation set demonstrated an impressive AUC of 0.915, underscoring the HCC Validator’s effectiveness in enhancing accuracy. Receiver operating characteristic (ROC) curves were plotted to evaluate the discriminative ability of the HCC Validator, further affirming its capabilities.
Case studies reveal that medical organizations utilizing the HCC Validator have achieved better financial outcomes and enhanced patient care, particularly within value-based payment models that tie reimbursement to quality and cost performance. Experts stress the importance of training providers on documentation requirements for effective risk adjustment, with the HCC Validator playing a crucial role in this educational endeavor. As Linghong Wu articulated, “The aim of this study was to develop and internally validate an interpretable machine learning model for predicting the risk of hepatocellular carcinoma in patients with chronic hepatitis B infection,” emphasizing the significance of advanced technology in risk assessment.
With features designed to streamline workflows and ensure compliance, the HCC Validator stands out as an essential tool for healthcare providers aiming to enhance their documentation practices according to MEAT coding guidelines. By addressing the specific challenges faced in HCC classification, the HCC Validator not only supports compliance but also empowers organizations to maintain accuracy and efficiency in their classification efforts. Ultimately, this leads to improved risk adjustment strategies through multidisciplinary collaboration and data-driven methods.
The Claims Assistant from Inferscience revolutionizes HCC claims analysis by identifying overlooked HCC codes from prior billing cycles. Leveraging real-time claims data analysis, this tool empowers medical providers to proactively detect and address potential coding gaps before submission. This strategic approach not only streamlines claims management but also significantly enhances the revenue cycle by minimizing the risk of denials.
With nearly 50% of providers still relying on manual denial reviews, the automation provided by the Claims Assistant is essential for boosting efficiency and ensuring financial viability in medical operations. As Nicholas Sachs observes, ‘As we approach 2025, medical organizations must embrace a more advanced, technology-driven strategy for denial management.’
The Claims Assistant embodies this vision by automating the identification of coding gaps in line with the meat coding guidelines, thereby reducing dependence on manual processes. Moreover, similar to the findings from the case study on Robotic Process Automation for Claims Management, the Claims Assistant employs advanced technology to enhance claims management efficiency, allowing providers to focus on patient care while maximizing their revenue potential.
Inferscience positions itself as a trusted partner in the medical sector, ensuring that solutions like the Claims Assistant provide both efficiency and compliance, ultimately enhancing risk adjustment through AI and streamlined workflows. To discover how the Claims Assistant can transform your claims management process, request a demo today.
Precise HCC classification is crucial for enhancing Risk Adjustment Factor (RAF) scores, which significantly influence the funding healthcare providers receive from Medicare Advantage plans. Inferscience’s Claims Assistant conducts a real-time gap analysis on claims files, recommending HCC codes that may have been overlooked, thereby improving billing accuracy. By accurately capturing and documenting all relevant diagnoses, providers can secure reimbursements that truly reflect the complexity of their patient populations. This practice not only strengthens financial sustainability but also elevates the quality of care delivered to patients.
Some organizations record HCC conditions biannually to maintain a consistent revenue cycle, illustrating how regular and precise classification practices can directly affect financial outcomes. As the Centers for Medicare & Medicaid Services (CMS) continues to modify risk models, ensuring accurate HCC classification becomes increasingly vital for optimizing funding opportunities. With anticipated changes for 2025, including a slight decrease in Star Ratings due to policy adjustments, providers must prioritize accuracy in documentation to effectively navigate the evolving landscape.
For example, a medical organization that implemented robust classification practices, supported by Inferscience’s AI-driven solutions, reported a 15% increase in their RAF scores, resulting in significantly enhanced Medicare reimbursements. Such success stories underscore the tangible benefits of investing in precise HCC classification and the transformative impact of technology on healthcare risk adjustment.
Request a demo of Inferscience’s Claims Assistant to discover how it can enhance your HCC classification accuracy.
Common challenges in HCC classification encompass inadequate documentation, failure to capture all relevant diagnoses, and a misunderstanding of the meat coding guidelines. These issues not only obstruct compliance but also significantly impact the financial well-being of medical organizations, particularly concerning Medicare Advantage compensation.
To address these challenges, investing in comprehensive training for programming personnel is imperative. Studies indicate that organizations prioritizing staff education experience a notable reduction in errors. Furthermore, the US Bureau of Labor Statistics projects an 8% increase in demand for healthcare compliance officers by 2026, underscoring the critical need for skilled professionals in this field.
Regular audits are essential for identifying gaps in programming practices, enabling organizations to implement necessary adjustments. Additionally, utilizing advanced programming tools, such as Inferscience’s HCC Assistant—which provides real-time feedback and suggestions—can streamline the development process and enhance accuracy.
The incorporation of AI and natural language processing (NLP) technologies has the potential to revolutionize risk adjustment in medical care by optimizing HCC classification and enhancing Medicare Advantage funding. Safeguarding sensitive patient data remains a top priority, particularly in light of the increasing cyber threats targeting medical information.
By proactively addressing these challenges, medical providers can enhance their billing precision and compliance, ultimately maximizing their funding from Medicare Advantage agreements.
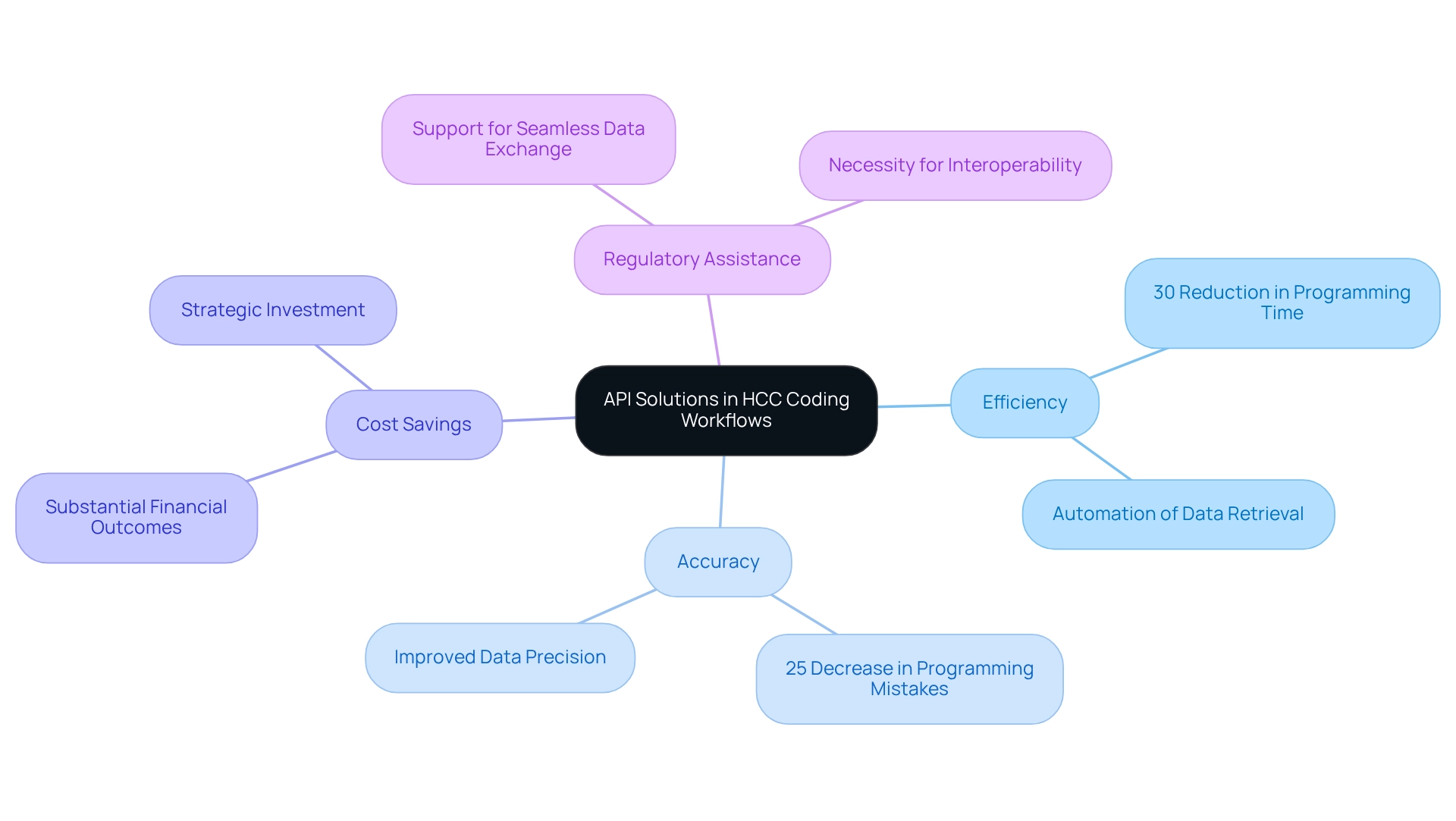
API solutions are essential for enhancing HCC documentation workflows by enabling seamless data transfer across various medical systems. The integration of APIs allows medical providers to automate the retrieval of patient data, ensuring that coders have access to the most current and relevant information. This automation accelerates the programming process and significantly mitigates the risks of errors associated with manual data entry, thereby enhancing accuracy and compliance.
As the European healthcare API market is projected to grow at a robust CAGR of 6.0% from 2025 to 2030, the demand for these solutions is driven by the increasing adoption of telemedicine, wearable devices, and advancements in AI-driven analytics. Case studies indicate that organizations leveraging API solutions alongside AI and natural language processing (NLP) have experienced notable improvements in workflow efficiency, including:
This underscores the transformative potential of these technologies in HCC classification, particularly in optimizing Medicare Advantage funding.
Furthermore, the emphasis on regulatory assistance for seamless data exchange underscores the necessity for interoperability in enhancing medical service delivery. By implementing API solutions, medical providers can not only streamline their programming processes but also elevate the standard of care through improved data precision and accessibility. As Brian Moore, VP at NICCA USA, Inc., remarked, “The quality of research they have done for us has been excellent,” reflecting the positive impact of API integration on healthcare workflows. For CFOs, these advancements can result in substantial cost savings and improved financial outcomes, positioning API solutions as a strategic investment.
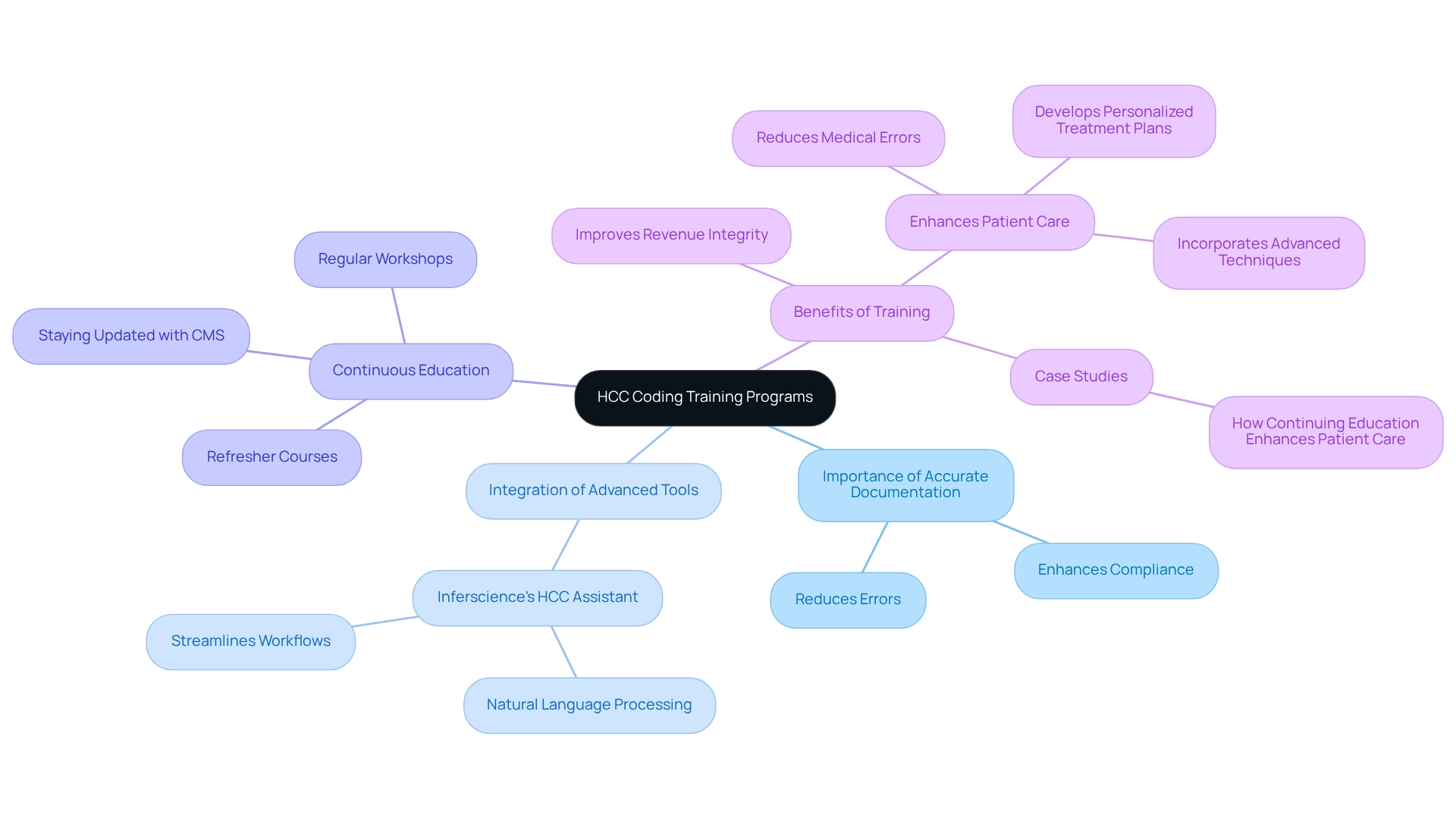
Implementing comprehensive training programs for programming personnel is essential to ensure adherence to HCC best practices. These programs must encompass the latest programming guidelines, underscore the importance of accurate documentation, and integrate advanced development tools such as Inferscience’s HCC Assistant. This intelligent tool employs advanced natural language processing (NLP) to streamline workflows, reduce manual effort, and enhance programming precision, ultimately optimizing Medicare Advantage funding.
Regular workshops and refresher courses are crucial to keeping staff informed about evolving regulations and programming practices. Ongoing education is vital for staying abreast of CMS announcements and industry changes. Data indicates that organizations investing in continuous training experience significant improvements in accuracy and compliance, ultimately enhancing revenue integrity and patient care.
Furthermore, expert insights highlight that continuous education not only reduces medical errors but also empowers providers to adopt evidence-based practices, leading to better patient outcomes. As Steve Barth notes, “With robust analytics, it offers transparent reporting, tracks performance, and ensures compliance, ultimately empowering your organization to enhance revenue integrity, maintain quality care, and confidently navigate the evolving risk adjustment landscape.”
Success stories from medical organizations illustrate that a commitment to staff training in HCC practices fosters a culture of excellence and accountability, ensuring that specialists possess the knowledge and skills necessary to navigate the complexities of the medical field effectively. Insights from the case study titled “How Continuing Education Enhances Patient Care” further demonstrate that ongoing education can decrease medical errors, develop personalized treatment plans, and incorporate advanced medical techniques, ultimately improving patient outcomes.
Artificial Intelligence (AI) and Natural Language Processing (NLP) tools are revolutionizing HCC classification by automating the extraction of critical data from clinical notes and electronic health records (EHRs). These advanced technologies excel at analyzing unstructured data, pinpointing relevant diagnoses, and recommending appropriate HCC codes in accordance with the meat coding guidelines. By harnessing the power of AI and NLP, healthcare organizations can achieve remarkable improvements in accuracy, significantly reduce the time spent on manual tasks, and bolster compliance with standards.
The integration of NLP tools not only streamlines risk adjustment workflows but also unifies patient data, addressing the common issue of data silos that can lead to inaccurate risk adjustment. Distinct characteristics of these NLP tools comprise their capability to examine extensive volumes of clinical data swiftly and precisely, guaranteeing that all pertinent patient information is taken into account during the documentation process. Recent advancements in AI tools have shown their effectiveness in improving programming accuracy. Engaging in collaborative efforts has resulted in an 18% improvement in patient satisfaction scores, as streamlined processes minimize wait times for services. Moreover, a significant segment of the public acknowledges AI’s potential to reduce ethnic biases in medical services, with 51% of U.S. adults endorsing its use for this aim. This viewpoint highlights the importance of AI in advancing fairness and enhancing medical service delivery.
Case studies have demonstrated that organizations using these technologies have experienced considerable enhancements in their risk adjustment outcomes, showcasing the transformative effect of AI and NLP on HCC classification precision and Medicare Advantage financing. As we look toward 2025, the landscape of HCC classification continues to evolve, with AI and NLP at the forefront of this transformation. Specialists in the domain highlight that the future of programming precision is encouraging, as these tools not only improve operational efficiency but also enable medical providers to concentrate more on patient care. However, it is essential to remain aware of challenges such as bias and ethical use that accompany these advancements. The incorporation of AI and NLP into HCC workflows is not merely a trend; it signifies a fundamental change in how healthcare organizations handle precision and compliance.
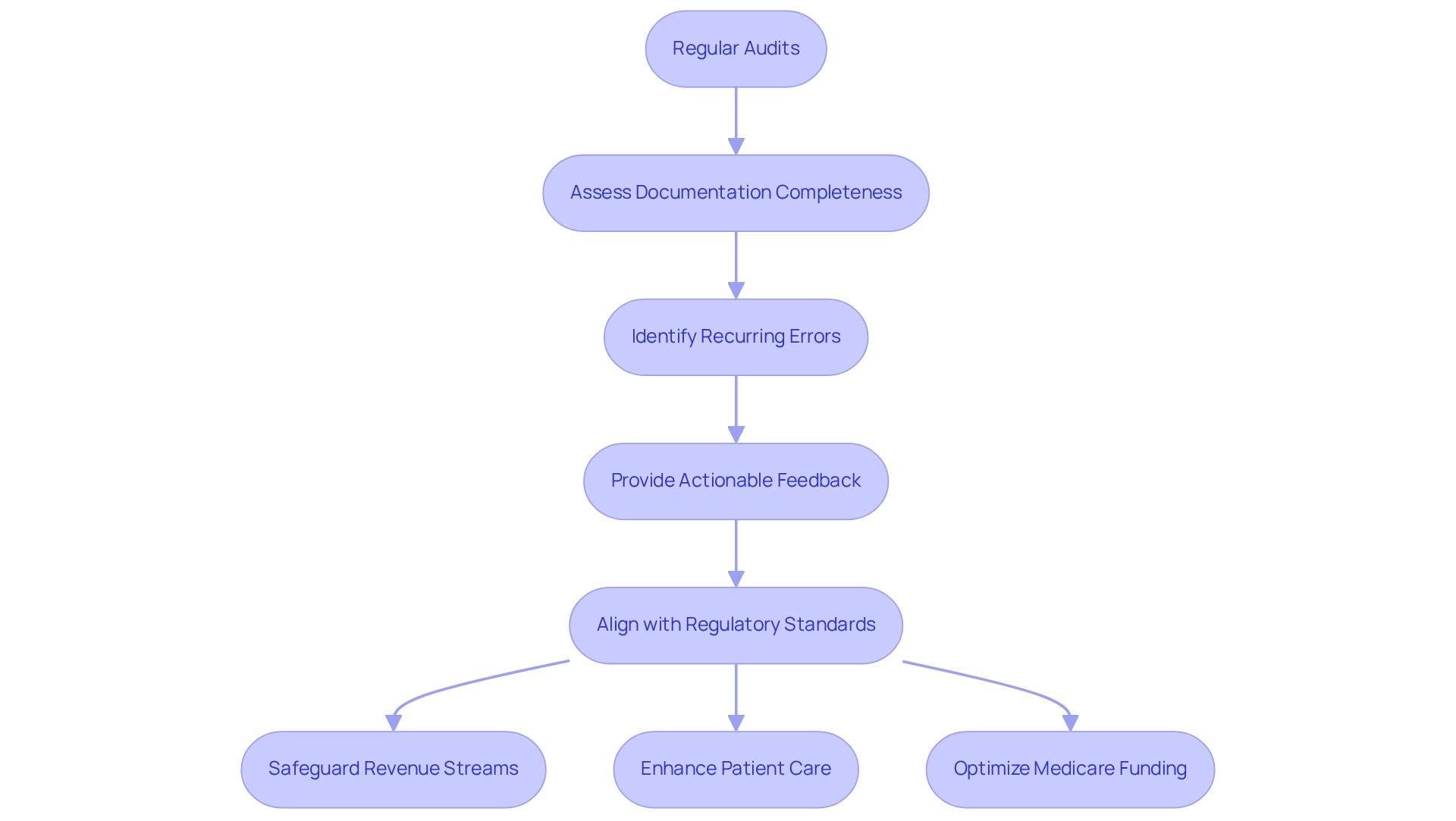
Regular audits of HCC documentation practices are essential for ensuring compliance and enhancing accuracy. These audits concentrate on assessing the completeness and accuracy of documentation, recognizing recurring error patterns, and providing actionable feedback to staff involved in programming. A well-organized auditing process not only aligns programming practices with regulatory standards but also safeguards revenue streams and enhances patient care results.
Inferscience’s AI-driven HCC classification solutions play a crucial role in transforming medical risk adjustment by streamlining workflows and reducing human error. Statistics indicate that potential recoveries from extrapolated audit findings could reach $4.7 billion by 2032, underscoring the significant financial implications of effective auditing. Furthermore, a case study from the Office of Inspector General (OIG) revealed that in 97% of cases with identified discrepancies, payers or medical groups did not contest the findings, suggesting a systemic acceptance of documentation errors. This highlights the necessity for rigorous audits to challenge and rectify such issues.
Expert insights underscore that regular audits are crucial in preserving programming precision. Compliance auditors emphasize the significance of posing challenging inquiries to reveal underlying problems, guaranteeing that healthcare organizations remain vigilant in their documentation practices. As Austin Barrington aptly states, “Ask the tough questions. We’re ready for them.” Success narratives from entities that have conducted regular audits showcase substantial enhancements in data precision and adherence, ultimately resulting in improved financial well-being and better patient care. CFOs should prioritize regular audits as a strategic method to enhance accuracy and compliance, utilizing Inferscience’s innovative tools to optimize Medicare Advantage funding. Additionally, insights from our FAQs highlight the importance of continuous education and training for coding personnel, ensuring they are equipped with the latest guidelines and best practices.
The integration of advanced technologies, such as artificial intelligence and natural language processing, is fundamentally reshaping the landscape of HCC coding, rendering it more efficient and accurate than ever before. Tools like the Inferscience HCC Assistant streamline the coding process by delivering timely suggestions and automating data analysis. This not only alleviates administrative burdens but also significantly enhances patient care. By adhering to the MEAT criteria and leveraging innovative solutions, healthcare providers can elevate documentation quality, effectively capture all relevant diagnoses, and optimize Medicare Advantage funding.
Challenges in HCC coding, including inadequate documentation and misunderstandings of guidelines, can be effectively addressed through comprehensive training programs and regular audits. These practices ensure that coding staff are thoroughly equipped to navigate the complexities of coding standards, ultimately leading to improved compliance and favorable financial outcomes. Moreover, utilizing tools such as the HCC Validator and Claims Assistant can mitigate risks associated with coding errors and enhance claims management, thereby bolstering the financial sustainability of healthcare organizations.
As the healthcare industry continues to evolve, the significance of accurate HCC coding cannot be overstated. By embracing technology and prioritizing education, healthcare providers can not only maximize their funding opportunities but also deliver superior care to patients. The future of HCC coding lies in the successful integration of these advanced tools and practices, which will be crucial for maintaining accuracy, compliance, and ultimately, the financial health of healthcare organizations in an ever-changing landscape.