Overview
The article outlines four essential steps for conducting an effective risk adjustment review, emphasizing the critical importance of accurate documentation, collaboration among healthcare staff, and the strategic use of technology to enhance coding practices. It details how comprehensive preparation, execution, and analysis of findings can lead to improved compliance and financial outcomes for healthcare organizations, particularly in light of upcoming regulatory changes from CMS. By implementing these steps, organizations position themselves to navigate the complexities of the healthcare landscape with confidence and efficacy.
Introduction
In the intricate realm of healthcare finance, the significance of risk adjustment is paramount. This statistical process is essential in shaping payment structures for health plans, reflecting the health status of enrollees. As we approach the transformative changes set forth by the Centers for Medicare & Medicaid Services (CMS) in 2025, grasping the fundamentals of risk adjustment is crucial for healthcare organizations aiming for compliance and precision.
Navigating the complexities of risk scores, Hierarchical Condition Categories (HCC), compliance requirements, and care gaps presents considerable challenges. As healthcare providers gear up for these developments, harnessing advanced technologies and implementing best practices will be vital for executing effective risk adjustment reviews. This proactive approach not only enhances patient care but also drives improved financial outcomes.
Understand Risk Adjustment Fundamentals
The risk adjustment review is a statistical process that adjusts payments to health plans based on the health status of their enrollees. Understanding its key elements is vital for effective risk adjustment review evaluations.
- Scores: These figures, derived from patient demographics and clinical information, represent the expected healthcare expenses for each individual. In 2025, the Centers for Medicare & Medicaid Services (CMS) will enforce stricter auditing regulations to combat upcoding in Medicare Advantage, making a risk adjustment review for precise score calculations more critical than ever. Inferscience’s solutions, particularly its advanced NLP tools, assist organizations in consolidating patient data and managing these changes, ensuring compliance and accuracy in classification practices.
- Hierarchical Condition Categories (HCC): HCC classification organizes patients based on their diagnoses, directly influencing scores and reimbursement rates. Real-world examples demonstrate that accurate HCC classification, bolstered by Inferscience’s HCC Validator, is essential for a risk adjustment review and can significantly enhance funding from Medicare Advantage contracts, underscoring its importance in financial planning for healthcare organizations. By leveraging AI-powered tools, healthcare providers can streamline workflow processes and reduce manual efforts, ultimately improving documentation accuracy, which is essential for a thorough risk adjustment review. Organizations should conduct internal audits, educate providers on diagnosis coding, and stay informed about CMS and Office of Inspector General (OIG) developments as part of their risk adjustment review to prepare for the upcoming CMS-HCC 2025 updates. Inferscience’s commitment to data protection, evidenced by its SOC2 Type II certification, positions it as a reliable partner in ensuring compliance and dependability in healthcare technology.
- Care Gaps: Identifying care gaps is crucial in modifying care, as they indicate instances where patients have not received necessary treatment, impacting their health outcomes and associated costs. For instance, a patient with diabetes may not have undergone an HbA1c test in the past year, a critical component for managing their condition. Addressing these gaps can lead to improved patient care and more accurate financial adjustments, which underscores the importance of a risk adjustment review, as Bob Herman, a Business of Health Care Reporter, emphasizes that understanding the financial implications of these modifications is vital for healthcare organizations. By familiarizing themselves with these essentials, they will establish a solid foundation for conducting effective evaluations, ultimately resulting in enhanced precision and compliance in healthcare payments.
Prepare for the Risk Adjustment Review Process
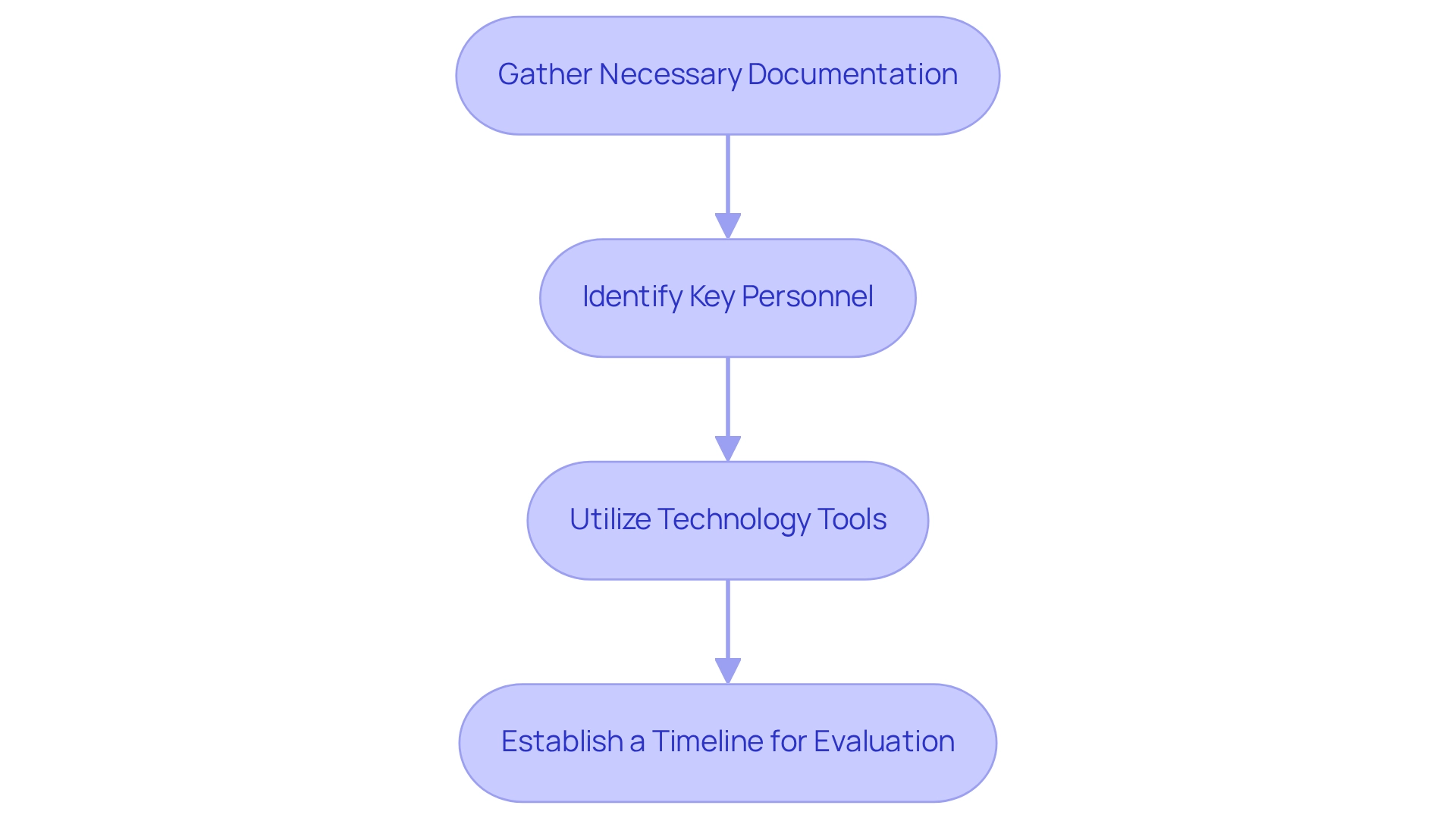
To efficiently prepare for a review of variations, consider the following steps:
- Gather Necessary Documentation: Compile comprehensive patient records, including medical histories, treatment plans, and prior coding documentation. Precise documentation is essential; statistics indicate that healthcare documentation errors can lead to a 30% decline in outcome modifications by 2025.
- Identify Key Personnel: Form a dedicated team comprising coders, compliance officers, and clinical staff. This collaboration is crucial for a thorough risk adjustment review, as diverse expertise ensures that all aspects are addressed.
- Utilize Technology Tools: Implement advanced software solutions, such as Inferscience’s HCC Assistant, which analyzes structured and unstructured data from patient charts and provides relevant HCC suggestions at the point of care. This seamless EHR-integrated platform not only automates data gathering but also enhances coding accuracy, streamlining workflows and allowing your team to focus on patient care while maximizing funding opportunities. The Milliman MedInsight Risk Adjustment Platform has demonstrated that streamlined processes and enhanced data accuracy can significantly improve decision-making and patient care outcomes.
- Establish a Timeline for Evaluation: Create a clear schedule that details each stage of the evaluation process. This guarantees that all team members are coordinated and accountable, promoting a seamless and effective assessment.
By adhering to these best practices, you can lay the groundwork for a successful risk adjustment review, ultimately leading to better HEDIS scores and improved quality of care. A meta-analysis of 24 studies utilizing machine learning for ADR prediction revealed that these technologies can achieve a weighted average accuracy of 72%, with certain models exceeding 80% sensitivity, underscoring the importance of employing technology in your evaluation process. Additionally, upcoming metrics in patient safety analytics may include preventable harm prediction accuracy and risk-adjusted safety profiles, emphasizing the necessity for comprehensive documentation and assessment.
Execute the Comprehensive Risk Adjustment Review
To effectively execute a comprehensive risk adjustment review, organizations must adhere to the following steps:
- Conduct a Chart Review: Scrutinize patient charts for accuracy in documentation and classification. Identify any missing diagnoses or discrepancies between clinical notes and coded data, as these can significantly impact Risk Adjustment Factor (RAF) scores. Leveraging Inferscience’s HCC Assistant can streamline this process by analyzing structured and unstructured patient data, ensuring that no critical information is overlooked.
- Cross-Reference with HCC Guidelines: Ensure that all documented conditions align with HCC classification guidelines. This alignment is essential for maximizing vulnerability scores and ensuring compliance, particularly in light of the latest CMS-HCC updates. Inferscience’s automated analytics enhance this process, providing real-time insights that support accurate coding.
- Engage Clinical Staff: Foster collaboration with physicians and clinical staff to clarify any ambiguities in documentation. This engagement is crucial for capturing all pertinent diagnoses, enhancing classification accuracy, and improving overall patient care. As Anita Schmidt, an AHIMA-approved ICD-10-CM/PCS trainer, emphasizes, precise coding is vital for effective modification and compliance. Inferscience’s tools facilitate this collaboration by integrating seamlessly into clinical workflows.
- Document Findings: Maintain thorough records of any discrepancies discovered during the assessment. Include recommendations for corrections and outline follow-up actions to ensure that all issues are addressed promptly. By utilizing Inferscience’s Claims Assistant, organizations can conduct a risk adjustment review through gap analyses on claims files, recommending HCC codes that might have been overlooked, thereby enhancing billing precision.
By diligently executing these steps, organizations can improve their evaluations, ensuring thoroughness and compliance. Statistics indicate that organizations adopting structured chart evaluation processes can significantly enhance their documentation completeness rates by up to 30% and coding accuracy percentages by 25%. This ultimately results in improved financial outcomes. Furthermore, leveraging technology solutions like Inferscience’s HCC Assistant streamlines these processes, allowing healthcare providers to focus on patient care while maximizing funding from Medicare Advantage contracts. Inferscience’s commitment to data security, demonstrated by their SOC2 Type II certification, underscores the importance of compliance and effectiveness in evaluations.
Analyze Review Findings and Implement Changes
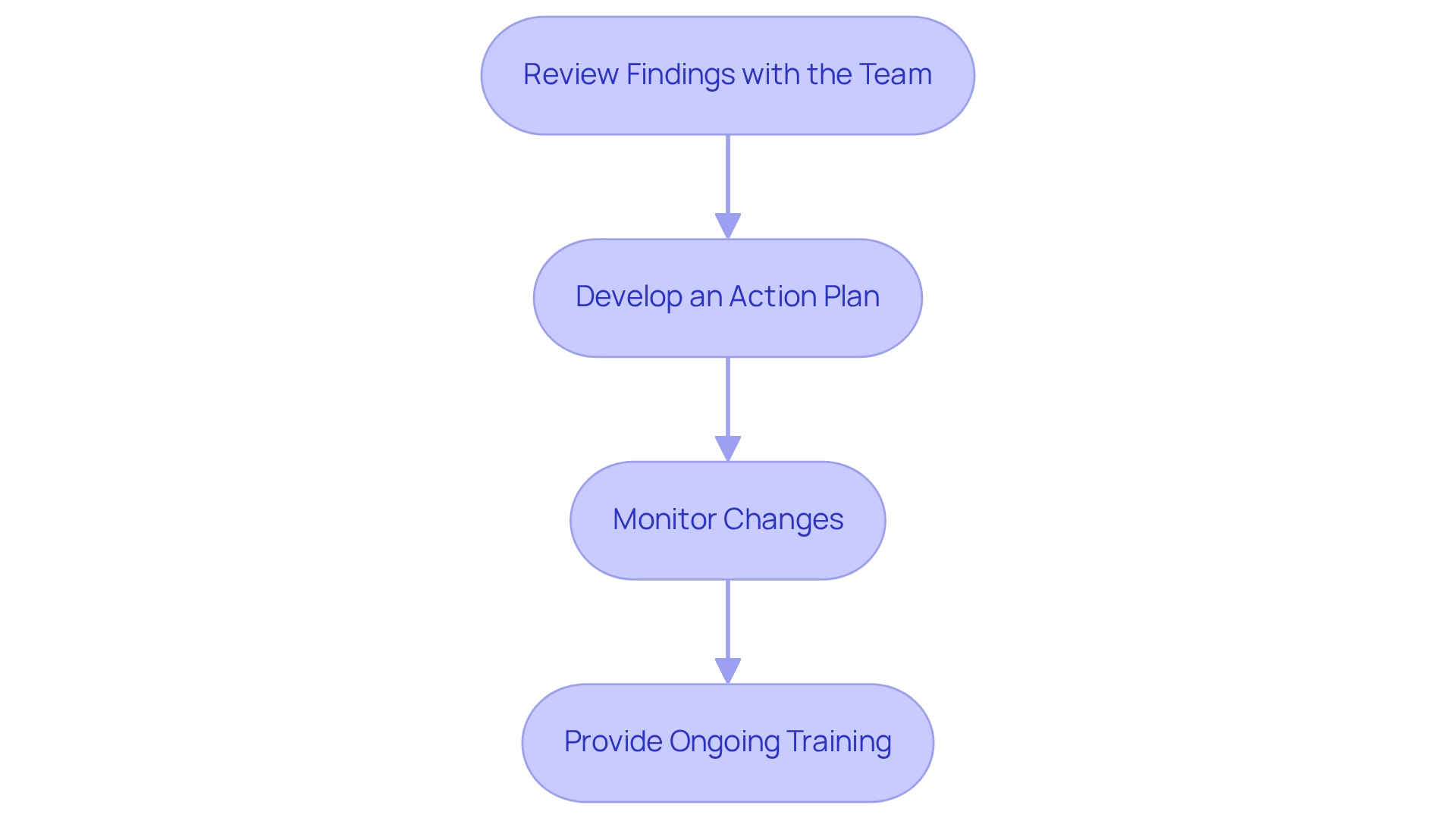
After completing the risk adjustment review, it is essential to systematically analyze the findings and implement effective changes. Here are the steps to follow:
- Review Findings with the Team: Organize a meeting with your team to thoroughly discuss the findings. Emphasize areas requiring immediate attention and improvement, ensuring that all team members understand the implications of the results. Leveraging tools like Inferscience’s Claims Assistant can facilitate this process by providing real-time analysis of claims data, suggesting HCC codes that may have been overlooked, thus enhancing the accuracy of your discussions.
- Develop an Action Plan: Formulate a comprehensive action plan that specifies necessary changes to programming practices, identifies training needs, and establishes clear timelines for implementation. This plan should be tailored to address the unique challenges identified in the risk adjustment review. As Rajeev Suri aptly stated, “Leadership is all about emotional intelligence. Management is taught, while leadership is experienced,” highlighting the importance of guiding your team through these changes. Incorporating AI and NLP solutions can further enhance your programming practices and streamline workflows.
- Monitor Changes: Create a robust monitoring system to evaluate the effectiveness of the implemented changes. Regularly assess programming accuracy statistics to ensure enhancements are maintained over time, allowing for prompt adjustments if necessary. Keep in mind that the average Medicare Advantage plan will have to submit proposed 2025 plans to CMS by June 3, 2024, making it essential to stay ahead of compliance requirements. Employing advanced analytics can provide insights into programming accuracy and assist in pinpointing areas for further enhancement.
- Provide Ongoing Training: Conduct regular training sessions for programming staff to keep them informed about best practices and any changes in regulations. Ongoing education is essential for upholding high standards in programming accuracy and compliance. Referencing case studies, such as the ‘Star Ratings Updates for CY 2025,’ can offer valuable insights into how CMS updates influence modification processes and the significance of adapting to these changes. Furthermore, training on the use of AI-driven tools can empower your team to utilize technology effectively in their programming practices.
By diligently analyzing your review findings and executing these steps, you can significantly enhance your risk adjustment review processes, ensuring alignment with Medicare guidelines and improving overall coding practices.
Conclusion
Understanding and implementing effective risk adjustment practices is crucial for healthcare organizations as they prepare for the upcoming changes mandated by CMS in 2025. The essential components of risk adjustment—risk scores, HCC coding, compliance requirements, and the identification of care gaps—play a significant role in shaping accurate payment structures and enhancing patient care.
Preparation for risk adjustment reviews necessitates gathering comprehensive documentation, assembling a skilled team, utilizing advanced technology, and establishing clear timelines. These steps are vital for ensuring that the review process is thorough and that coding practices are accurate and compliant. Moreover, executing a comprehensive review requires diligent chart analysis, collaboration with clinical staff, and meticulous documentation of findings, all of which contribute to improved financial outcomes.
Analyzing the review findings and implementing necessary changes is a continuous process that demands regular monitoring and ongoing training. By fostering a culture of learning and adaptation, healthcare organizations can enhance their coding accuracy and compliance, ultimately leading to better patient care and financial performance. Embracing these practices not only prepares organizations for the future but also positions them to thrive in an evolving healthcare landscape.